Addressing Dementia: How to detect, evaluate and approach suspected cognitive impairment
By: Jennifer Pilcher, Ph.D., CMC
Talking about dementia can be hard and scary. However, learning about the common symptoms, the difference between dementia and normal aging, and what you can do if you get a diagnosis of dementia can help to alleviate fear and help you be more prepared to address this issue for yourself, a client or a family member.
What is the difference between normal aging and dementia?
It is important to understand and acknowledge that there is a difference between Normal Aging and Dementia. As people age, there are several changes that occur in the brain that are related to the normal aging process including:
- Takes longer to encode, store, and retrieve information
- Rate at which new information is learned is slower
- Greater need for repetition
- Long and short- term memory changes
- Word finding ability declines
- Abstraction and mental flexibility shows some decline
Dementia, on the other hand, has symptoms that are above and beyond what we would expect to see in a normal aging process. Dementia is not a disease itself, it’s a syndrome or a description of a collection of symptoms.
The symptoms of dementia can include increased confusion, short term memory loss, poor judgment, difficulties with language and word finding, visual-spatial reasoning and changes in mood including: paranoia, suspicion, depression, anxiety and agitation.
The important distinction between normal aging and dementia are two things:
- Most people with cognitive changes related to normal aging are able to use compensatory strategies such as making lists or using a calendar to manage the changes.
- People with dementia, on the other hand, they are less likely to be able to use these strategies independently. Most importantly, the changes they are experiencing are interfering with their ability to function in regular life and having a serious impact on their lifestyle.
What causes dementia?
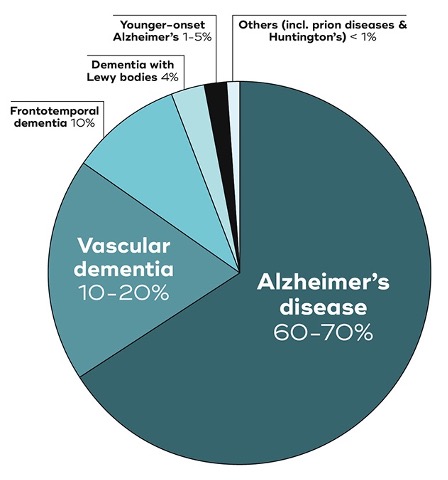
The most common cause of dementia and the one most people are familiar with is Alzheimer’s disease. Alzheimer’s alone makes up to 70% of dementia cases. Alzheimer’s disease systematically shrinks and destroys many of the areas of the brain. The cortex shrivels up, the ventricles grow larger and the hippocampus shrinks which is a key area of the brain that allows us to store memories. In fact, there are actually over 20 different variants of these diseases that can cause dementia. These other variants include Vascular Dementia, Frontotemporal Lobe Dementias, Lewy Body Dementia and many others.
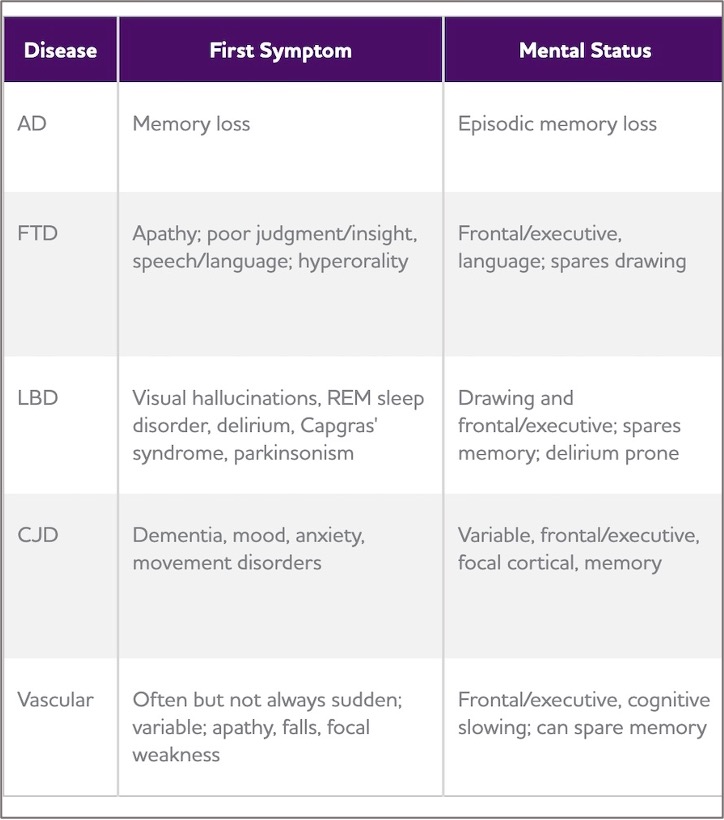
Recognizing that there are other causes of dementia is important because these variants present very differently. Pretty much everyone knows at this point that the first and most prominent symptom of dementia caused by Alzheimer’s disease is memory loss. However, the non Alzheimer’s dementias have very different initial symptoms that may be overlooked or misinterpreted if you aren’t aware of them. For example, people with Frontotemporal Lobe Disorders may appear withdrawn, experience personality change or have issues with their language. People with Lewy Body Dementia have hallucinations, sleep disorders and Parkinson’s like symptoms. People with Vascular Dementia often have issues with executive functioning and cognitive slowing as well as apathy and falls. For many of these atypical dementias, if you didn’t know better you might suspect depression, mid life crisis or substance abuse. It can be very difficult for people who have these variants to get a diagnosis.
Importance of Medical Evaluation
If you or someone you know is experiencing any of these symptoms, it is important that you first pursue a medical workup to rule out other reasons for the symptoms you are having. There
are several illnesses that are not dementia, but have dementia-like symptoms. Depression can often have symptoms that look like dementia, but are actually treatable. As well, there are metabolic and organic changes or illnesses that could create dementia-like symptoms but are actually reversable. It is vitally important to rule out these other causes of these symptoms before assuming a person is experiencing dementia.
How is a Diagnosis of Dementia Made?
There are a series of imaging and other tests, including blood tests that can now help neurologists to narrow down which disease a person may be experiencing. Both MRI and PetScan are routinely used to identify changes that are not related to normal aging, but also to identify what part of the brain is being affected. Lastly, a lumbar puncture is now routinely being done to rule out or rule in Alzheimer’s disease.
However, the imaging that is done is only half of the diagnostic process. Additionally, the neurologist takes a thorough patient history and extensive interviews with the patient’s family or friends. These interviews are combined with a battery of tests that are called neuro – psychological testing. This testing usually takes a few multiple hour sessions to complete. If you or someone you know are experiencing symptoms of dementia, it is vitally important that they have this testing done.
Despite the fact that we have these two systems for determining a diagnosis, it can still be quite difficult to get a diagnosis, especially if you are experiencing symptoms of one of the atypical dementias.
Differential diagnosis and why it is important
It is important not just to have a neurologist determine that you are experiencing symptoms of dementia, but also to be able to identify what kind of dementia you are experiencing. This is called getting a “differential diagnosis”. Part of the reason that a diagnosis of atypical dementia is difficult to get is that the routine screening mechanisms we use are not set up to detect the symptoms of atypical dementias. There are several screening tools that are typically used for this purpose. For example, the Mini Mental Status Exam (MMSE) or The Montreal Cognitive Assessment (MOCA). These tools are created to detect changes in several different kinds of memory and executive functioning. However, they are not able to assess judgment, impulse control, personality change, and/or rational thinking, all of which are common signs of atypical dementias such as Frontal Temporal Lobe Dementia. A patient can have a decent score on one of these screening tools but still be experiencing dementia. For this reason, if you are experiencing a non-Alzheimer’s dementia, it may take several visits to the neurologist 6 months 3 years to get a differential diagnosis.
Getting a differential diagnosis is important for two reasons:
- Because these atypical dementias are so different, they are also treated differently both pharmaceutically and non pharmaceutically. Some of the medications that neurologists would use to treat one dementia could actually exacerbate the symptoms of another.
- Getting a differential diagnosis can help the caregiver understand the brain science behind what is happening and that the behaviors the person is exhibiting are not intentional, but rather disease related. This explanation can go a long way to avoiding caregiver burnout.
But How Do We Talk About It?
Thus far, we have discussed how to recognize your client or their family member may have a cognitive impairment and what the diagnostic process looks like.
Next we need to talk about how to talk with your Client or the family about your concerns.
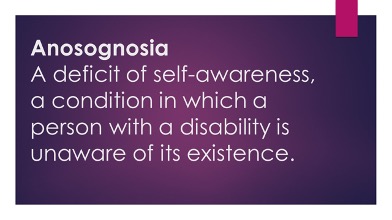
This is tricky business. The first thing to know is that almost all people with dementia have a symptom called Anosognosia: a lack of insight or awareness of their impairment, the severity of their impairment or how their impairment impacts their daily life. For people who have this symptom, it is virtually impossible to have a rational and straightforward conversation with them about their illness or potential illness. In some ways, this is seen as a protective measure for the person with the illness. But for caregivers or those trying to get the person evaluated or more support as they need it, this is really difficult. It is important to acknowledge this is NOT denial, this is true lack of awareness. If you are seeing potential signs of cognitive impairment, it is very important for you to understand and explain to your client’s family that that the person with the impairment may not be able to acknowledge the illness no matter what you say.
Given that lack of insight is an issue, how do you talk with your clients about the concerns you or they are observing?
- Reassure the client or family member that many people experience changes in cognition as they age.
- Ask questions, ask the client or family member to give details about their symptoms and how or if these symptoms are interfering with their daily life.
- Ask these questions separately to the client and the caregiver and watch for difference in reports.
- Whatever you say, don’t use the “word” dementia. Talk about symptoms, not labels. Refer to symptoms the person themselves have talked about experiencing. Rather than saying. “If you are worried you have dementia, you should see a doctor”. You would say “For other clients of mine who have experience memory loss/cognitive changes/difficulty with attention, I have suggested the following……..”
The key to a successful conversation is to reflect back what the client and/or their family members are reporting without creating more fear.
Other Talking Points
Educate about Causes
Previously we discussed what causes dementia. However, there are other illnesses that can cause dementia-like symptoms that are not actually a result of dementia. For example, things like depression, delirium or even dehydration in extreme cases can cause dementia-like symptoms.
When I am speaking to a family and/or the client about the need for testing, I am often pointing out that it is possible their symptoms are being caused by something that is treatable and that it would be a shame if we didn’t know that. This is often something that both clients and their family members can hear and will help motivate them to seek out evaluation. A person experiencing symptoms should get a full medical workup in order to rule out organic or metabolic causes.
Early Detection
Pointing out the importance of early detection is another way to approach this subject.
At the current time, although we have some medications that can slow the progression of the dementia and treat the common side effects of these diseases, there is no prevention or curative treatment. However, early detection of these diseases is critically important for a few important reasons.
First. research has shown that there is a pre-clinical phase of dementia where the patient is not experiencing any symptoms. This phase can be up to 10-15 years before the person is showing symptoms we can identify. Our detection has gotten better over the years. In the past, we could only recognize symptoms of cognitive decline when a person had fully developed Alzheimer’s disease. Now we are able to recognize a syndrome called Mild Cognitive Impairment (MCI), which is often a precursor to developing Alzheimer’s disease.
Second, much of the research about the medications we have available to treat dementia today are believed to be more effective the earlier you receive them in the
process of the disease. In fact, there is a common belief among the developers of these drugs that they would be more effective if they were given in the pre-clinical stage of the illness.
Lastly, there are things we can do to address both the progression of the illness and the common symptoms. For example, we can provide interventions to help with:
- Communication with Speech Pathologists
- Physical and motor issues with Physical and Occupational Therapists
- Diet and lifestyle
- Cognitive strengthening and training
- Avoiding social isolation, depression and anxiety
- Adjusting estate plans and creating documents
Solo Conversations with Caregiver
Keeping the client’s lack of insight in mind, it may be very important for you to have a 1:1 conversation with the well family member to reinforce or introduce ideas you may have mentioned in a group setting. This is important even if the client appears to have insight about their symptoms and is willing to address or evaluate it. You may need to give the family member more information about the reasons for getting a full neuro psychological workup to determine if what they are seeing is a result of normal aging or a disease process.
It is important to talk to the caregiver about the fact that it will take time to get a differential diagnosis and that they may have to push for more definition over time if symptoms don’t resolve. Getting a differential diagnosis can also help the family member understand the symptoms of the illness and allow them to learn strategies for addressing the symptoms. Most importantly, this will help the caregiver to understand the behavior is not intentional and to plan supports accordingly.
Lastly, it is essential to speak to well family member alone about supports for themselves as they go through this process. The data on caregiving is not good. In one recent study 17% of caregivers reported that their health was either fair or poor – this is 7 percentage points higher than the general population average. In this same study 38% of caregivers reported feeling highly stressed due to caregiving responsibilities. Equally as shocking are the number of caregivers that predecease the person with dementia due to stress of caregiving. For these reasons, planning for both emotional and practical support is essential for the caregiver’s well being and survival.
Bringing in Other Professional Support
Once you have begun the conversation with a client and/or their family member about potential concerns, you may want to consider bringing in other professionals to help. Here are some examples of when it would be a good idea to do so:
- If a client or family member is seeking out education about dementia and how to get connected to a neurologist.
- If client is highly resistant to getting an evaluation or doesn’t acknowledge the problem
- If there are complicated family dynamics or co-mingling problems
- When the care or supervision of a person with dementia is getting difficult
- If the person you are concerned about is younger (-65 years old), a diagnosis like this can be financially devastating. (For this age group, there are many different implications for disability benefits and the need for Medicaid planning. This would be a good time to introduce an Elder Law Attorney if the client does not already have one).
Resources
Below are some resources you can utilize to find professionals that can be helpful.
For information about dementia and caregiver training/support
Alzheimer’s Association (https://www.alz.org/manh)
The Dementia Care Collaborative (https://dementiacarecollaborative.org/)
To search for an Elder Law Attorney in your area:
https://www.naela.org/findlawyer
For help with caregiver education, resistance to evaluation or care, complicated family dynamics or co-mingling problems or for problem solving when the care of supervision of a person with these symptoms is getting difficult, consult an Aging Life Care Professional in your local area: